30 percent of people under the age of 65 have a chronic health condition. Despite this prevalence, people with chronic illnesses or disabilities often face discrimination. Over a third of disabled people have experienced negative bias in their current job. The unemployment rate is twice as high for people with disabilities, compared to the general population, even though companies which are inclusive of people with disabilities are more financially successful. People with disabilities earn significantly less than non-disabled people with the same education level. While there is a dearth of data specific to the tech industry (major tech companies gave evasive, off-the-record answers when asked by a disabled reporter why they don’t include disability in their diversity reports), there are plenty of first-hand accounts of exclusion and bias.
Because I occasionally tweet about my health struggles, (which include two brain surgeries, a life-threatening brain infection, and two ICU stays), a number of people in the tech industry have contacted me to privately share about their own experiences with disability or illness. Many of them say that they fear discrimination within the tech industry if they were to speak publicly about their health. Will people think that I’m less capable? Will my manager be less likely to give me important and high impact assignments? Will this change the lens through which people view my achievements or productivity? Sadly, these fears can be well-founded.
The people who build technology need to be representative of the people who use that technology, which increasingly includes everyone. Some of the users of your product have chronic illnesses and disabilities (whether you realize it or not) and they need to be involved in the creation of your product. In this 2-part set of posts, I want to address some misconceptions about disability, and to offer advice on how to improve, both in our interpersonal interactions and in our work cultures.
The disability pay gap, unemployment, and job loss
Haben Girma, the first deafblind person to earn a law degree at Harvard, wrote of her experience of discrimination, even as a high achiever who excelled at school and work, “Hard work alone will not overcome the widespread discrimination against people with disabilities. Employers need to break down disability barriers. People with disabilities succeed when communities choose to be inclusive. The biggest barriers exist not in the person, but in the social, physical, and digital environments.” (emphasis mine)
Data from the UK shows that “the disability pay gap — the difference between what non-disabled and disabled workers earn — is 13.6 percent. On top of that, disabled people are significantly more likely to be unemployed, lose a job and be in low-waged work than non-disabled people. We’re also routinely given fewer responsibilities at work and turned down for promotion, or refused the job in the first place.” In the USA, there is a disability pay gap at all educational levels, which grows greater for higher levels of education.
Many tech companies have explicit reputations as being unwelcoming to those with health issues. At Amazon’s headquarters, multiple employees were given low performance reviews or put on performance improvement plans (a precursor to being fired) after having cancer or major surgeries, as reported in a 2015 New York Times article. “A woman who had thyroid cancer was given a low performance rating after she returned from treatment. She says her manager explained that while she was out, her peers were accomplishing a great deal… A woman who had breast cancer was told that she was put on a ‘performance improvement plan’, because ‘difficulties’ in her ‘personal life’ had interfered with fulfilling her work goals… A former HR executive said she was required to put a woman who had recently returned after undergoing serious surgery, and another who had just had a stillborn child, on performance improvement plans.” (emphasis mine) While being fired immediately after cancer treatment or surgery is particularly egregious, bias often shows up in more subtle, yet still harmful, forms, such as: not accommodating medical or scheduling needs; inaccessible buildings or processes; inadequate HR resources; resentment towards a coworker that has taken medical leave; or even distrust/disbelief that someone’s experiences could be so different than your own.
The tech industry’s obsession with working ridiculously long hours is inaccessible to many disabled and ill people, for whom adequate rest is often not optional, or who may have regular doctor’s appointments, physical therapy, or tests. On top of being exclusionary, this insistence on long hours is contrary to research on productivity — it doesn’t even lead to more productive companies.
Health is not binary
Illness & disability can fluctuate. Perhaps some days a person needs a wheelchair or cane and other days they don’t. Some days they are capable of tasks that other days they can’t do. Google developer advocate, Julia Ferraioli, who has had a vision impairment off-and-on for the last two years, shared in her GopherCon keynote, that “Disability is not binary. There are some days when I can churn out code, and some when I can’t read anything at all.”
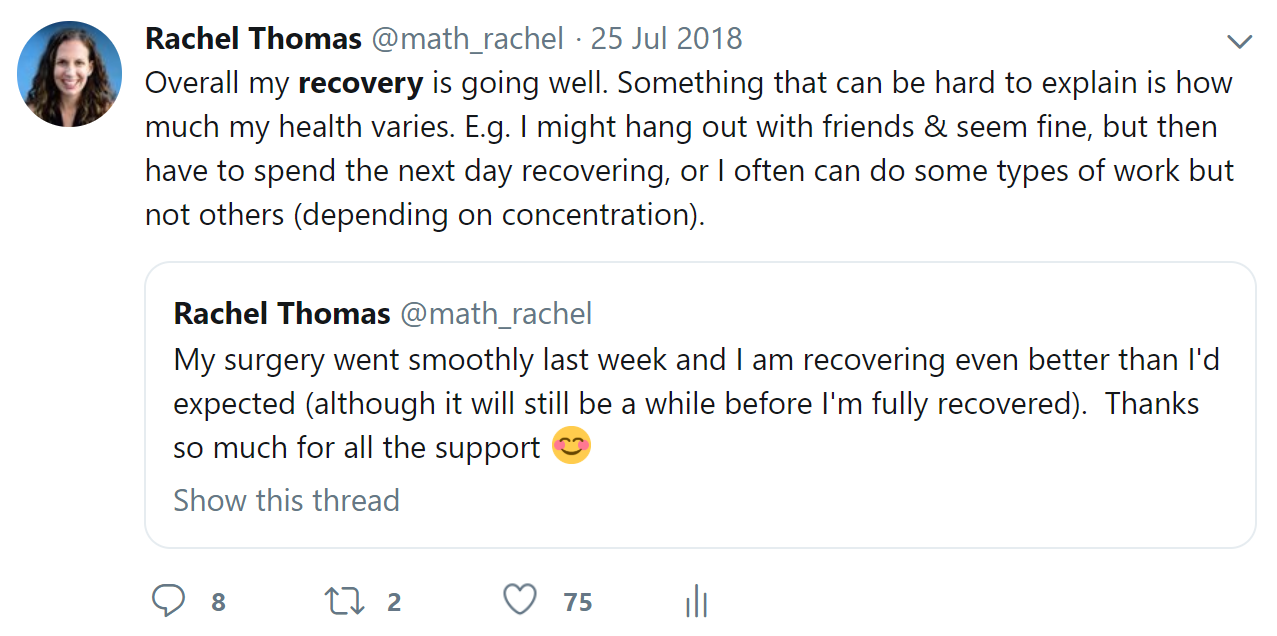
I have some dramatic stories of my most acute health crises, but what is harder for me to explain is the long stretches of time where my health was in-between — when I was not fully well, but could give high-profile talks (although it would take days to recover), attend conferences (even if just for a few hours each day), or teach (even if I felt awful and spent all my time outside of class resting). I hear similar accounts from many people whose symptoms fluctuate over time, or who experience flares alternating with periods of reduced symptoms. Even the recovery from a particular illness or surgery is rarely linear, and a better week may be followed by a worse week. Many people worry that if they share about their disability, people may accuse them of “faking it” if they are not perfectly consistent in their behavior.
Gabe Moses, who often uses a wheelchair and sometimes uses crutches, wrote a post addressing how wheelchair users are often wrongly accused of faking their disability. Gabe has unstable joints, unpredictable muscle spasms, and sudden numbness, which makes getting around without a wheelchair exhausting, painful, and dangerous (although possible, at least sometimes). He writes, “The black-and-white narrative of disability we’ve been sold makes people who haven’t experienced disability themselves see wheelchair users this way: wheelchair users are people who can’t walk, at all. Anyone else who dares to use one is either lazy or faking. The truth is, wheelchair users are a highly varied group of people. Some people do need their wheelchairs because of paralysis or other conditions that make walking impossible. Others use them because of fatigue, chronic pain, balance problems, or other conditions that make it impossible to walk long distances, even if they are capable of standing and walking to some degree.”
Illness & disability can be invisible
“You seem like you are doing great!” people tell me when I bring up my health challenges. Sometimes people who see me seeming upbeat during a social event or watch one of my talks assume that I must be fully recovered. Whereas in reality, it is common to feel ok at some times but ill at others (and this can vary from week to week, or even throughout a given day), to appear healthier than I feel inside (particularly if I’m trying to show my best side at a professional event), or to need an unusually long amount of time to recover from events where I seemed “normal”. People are complex and multi-faceted, and you can’t assess their health based on appearance or mood.
Product designer Amélie Lamont shared that while on disability leave from work, she spoke at the conference (after clearing it with her doctor and after having had to cancel her talk the previous year due to her health). It took her days to recover, yet her employer assumed since she seemed fine during the 30-minute talk, that she must be well enough to return to work full-time. In doing so, her employer was failing to understand that illness can be invisible, and that Amélie and her doctor are the only ones who can determine when she is actually ready to return to work.
To give one small personal example, at NeurIPS 2017, I attended interesting talks, mentored at two round table discussions for the Women in ML workshop (which inspired me to later write blog posts on personal branding and founding startups), and met many new people. At one point, I was one of the two top people recommended to follow for the #NIPS2017 hashtag. Unless I spoke about it, most people I talked to at the conference probably wouldn’t have guessed how unwell I was (I was recovering from a life-threatening brain infection, and had an infected brain cyst which would require an additional surgery), or that I only attended a few hours of talks or events each day, took breaks to lie down on the floor of the conference center, had daily headaches, and went to bed early each evening. This paints two different pictures of my time at the same event.
A friend, who has a disease which impacts her mobility, told me that at NeurIPS 2018 there were seats that were supposed to be reserved for people with disabilities, yet they were always full. Since my friend “looks healthy”, she felt too uncomfortable to ask someone else who “looks healthy” if she could have one of these seats; perhaps they have an invisible illness as well. She also felt unsure whether she even wanted other people in the AI community to know about her disability, as this would change how they view her.</p>
Trust people to understand their own bodies & experiences
Many people with illness and disabilities have spent years trying to get diagnosed, to get their symptoms taken seriously, to get treatments they needed approved or covered by insurance, or to get accommodations they need at work. For instance, a study in the UK found that almost a third of patients with a brain tumor had to visit a doctor more than 5 times before receiving their diagnosis (these times are longer for women and low-income patients). One woman with a brain tumor recalled: “One of the GPs I saw actually made fun of me, saying ‘what did I think my headaches were, a brain tumor?’ I had to request a referral to neurology. I went back repeated times to be given antidepressants, sleep charts, analgesia, etc. No one took me seriously.” On average, patients with autoimmune diseases have to visit 5 doctors over a 5-year period before receiving a proper diagnosis.
Research shows that doctors take the pain of women less seriously than the pain of men, and the pain of people of color less seriously than the pain of white people (resulting in longer time delays to receive treatment, lower quality of care, and worse outcomes). Since so many doctors were dismissive of her symptoms, it took author Aubrey Hirsch 6 years and a dozen doctors to get her Grave’s disease diagnosed. By that point, the disease had done permanent damage to her bones, heart, and eyes, which could have been prevented by earlier treatment. Hundreds of people responded to the powerful comic she created with their own experiences of having severe symptoms dismissed.
A few years ago, I went to the ER in the worst pain of my life, and was given no tests, but just sent home with aspirin (it turned out I actually needed brain surgery). Another time, I had not slept in days because of heart problems, and an ER doctor told me to “relax and take melatonin” when in reality my PICC line had been inserted 5cm too deep and was mistakenly inside my heart. I was once not believed about having dislocated my shoulder, which later resulted in my needing a surgery which my surgeon said could have been avoided if I had gotten treatment at that earlier time.
The trauma of the medical system
If you don’t have first-hand experience with chronic illness or disability, it can be difficult to understand how encompassing it can be. If you do not have first-hand experience trying to navigate the byzantine and traumatizing medical system, it can be surprising just how complicated, error-prone, and often hostile to patients<spa< span=””>n> it is. A growing body of research is linking medical trauma to PTSD.</spa<>
Liz Allen, who works in tech and has a complex range of immune issues, gives many reasons why she was hesitant to ask HR for the accommodations she needed, including that her story is long and traumatic to retell, educating others can be emotionally exhausting, she is often doubted or disbelieved, and her fear of being viewed as incompetent. Remember that it takes bravery for someone to share about their health with you; honor that and respond in a supportive and accommodating way.
Avoid giving unsolicited health advice.
Most people with chronic illnesses or disabilities have spent hundreds of hours researching their conditions, met with dozens of specialists, and tried a variety of treatments (both medical and lifestyle). Even when it’s well-intentioned, offering unsolicited health advice can come across as patronizing or dismissive. There is a huge amount of variety in different conditions and what works for different people, so avoid statements like “{yoga, x diet, physical therapy} is good for everyone.” Know that if a simple solution existed, the person would have already figured it out. Trust people to know their own bodies and to be experts on their own lives.
The limits of language
Don’t compare everyday experiences to someone else’s chronic condition. Feeling tired is not the same as chronic fatigue. Being sad is not the same as clinical depression. Doing Vipassana meditation for an hour is not the same as living with chronic pain for years. Part of this is a failure of language: words like “pain” and “fatigue” are used to describe a wide range of experiences. A friend with multiple sclerosis told me how regular fatigue (after a hike or long day) is very different from multiple sclerosis fatigue (which can involve nerve pain, muscle pain, and double vision), yet they are described with the same word, which leads to poor understanding. Brianne Benness, who has a chronic illness and started a podcast about chronic illness, also spoke about this limit of language, in response to an interviewee with epilepsy, Ehlers-Danlos syndrome, and cochlear implants, “I think I end up talking with people a lot right now about how we don’t have good words for what that feels like.” People who have never experienced severe pain may not be able to imagine what it feels like, yet it is still possible and necessary to practice empathy.
Medical Leave is not a “vacation”
Don’t tell someone that you wish you could spend the day in bed or take a month off from work like them — nobody wants to be in pain or suffering. Comparing medical leave to a “vacation” is dismissive of the pain, limitations, and actual work that go into medical leave. I also want to address the concern that an employee going on disability leave or requiring special accommodations results in extra work for their coworkers. If this does occur, it is not the fault of the ill or disabled person; it is the fault of the employer for not adjusting workloads, dropping lower priority tasks, or hiring additional temporary help (ditto for when child-free people are given extra work to cover for parents — this is the employer’s fault for not ensuring humane and fair work conditions for everyone). While the moral and legal cases for inclusion should be more than enough, note that companies that champion people with disabilities outperform other companies financially, with 28% higher revenues, 200% higher net income, and 30% higher profit margins.
Listen to other people’s experiences
Even if you don’t realize it, you are interacting with chronically ill and disabled people regularly. I hope the experiences, advice, and quotes shared in this post will be helpful in increasing empathy and understanding, so that we can make the tech industry more inclusive. I don’t and can’t speak for everyone with chronic illnesses or disabilities, so I hope that you will seek out and listen to the experiences of other people with chronic illnesses or disabilities (and the links in this post are one way to get started!)
This article was originally published on Medium by Rachel Thomas, a director of the USF Center for Applied Data Ethics and co-founder of Fast AI, a company which is making deep learning more accessible to people with little computational power and non-traditional backgrounds. She was selected by Forbes as one of 20 Incredible Women in AI, earned her math PhD at Duke, and was an early engineer at Uber.
Get the TNW newsletter
Get the most important tech news in your inbox each week.